
The Greifswald Newborn Screening Program screens newborns for metabolic and endocrine disorders identifying infants who need immediate treatment to prevent developmental problems, mental retardation or death. Identified infants are tracked to ensure they receive appropriate medical care. Approximately one out of every 1,400 babies is born with a disease detectable through Newborn Screening.
Newborn screening centre Mecklenburg-Vorpommern
Institute of Clinical Chemistry and Laboratory Medicine, University Medicine Greifswald
Ferdinand-Sauerbruchstr.
17475 Greifswald
Tel. +49-3834-865527, Fax +49-3834-867003,
Email: neugebscreen@uni-greifswald.de
It tests babies for serious disorders and is usually performed when your baby is 36-72 hours old. This test is often referred to as the "PKU test".
The test is done to find out if your baby has a disease or condition for which early treatment can prevent death, mental retardation, or physical disability.
The test is performed by pricking your baby's heel and putting a few drops of blood on a special filter paper. The paper is allowed to dry and then sent to the newborn screening laboratory where several different tests will be performed.
Parents who have no family history of problems and/or who have already had healthy children can still have children with these disorders. In fact, most children with these disorders come from families with no previous history of the condition.
Most babies with disorders look and act normal, and seem perfectly healthy. The newborn screening test helps your doctor to catch a problem with your baby before it gets sick. Most babies that are diagnosed and treated early live normal lives. The earlier the detection, the higher the chance of a normal life.
Basic screening
Condition (Incidence) | Analyte (Laboratory method) | Symptomes if not treated | Treatment |
Congenital Hypothyroidism lack of thyroid hormone 1:3,000 | TSH (Fluoroimmu-noassay) | Poor growth and mental retardation, other brain damage, growth delay | If found early and treated with thyroid medication, a child will grow and develop normally |
Congenital Adrenal Hyperplasia lack of an enzyme that the adrenal gland uses to process hormones. Analyte1:12,000 | 17-OH-P (Fluoroimmu-noassay) | Serious loss of body salt and water, even death, may occur to either sex. | Treatments are available to correct the condition (Glucocorticoid and/or mineralcorticoid) |
Galactosemia baby cannot break down the galactose part of milk sugar1:60,000 | (Enzymatic assay fluororescence measurement) | Severe brain damage, liver disease, cataracts; death
| Special milk-free diet prevents the problems. |
Biotinidase deficiency lack of an enzyme called biotinidase1:60,000 | (Enzymatic assay fluororescence measurement) | Mental retardation, seizures, skin rash, alopecia, hearing loss, death | Problems can be prevented with biotin treatment. |
Cystic fibrosis impaired transport of salt in and out of the gland cells 1: 3.300 | Up to 3-steps: Immunoreaktive trypsin, pankreatitis-associated protein/ Fluoroimmunoassay, DNA-analysis (31mutations) | Thick and sticky mucus in the lungs and other organs, chronic inflammation, reduced growth, significantly reduced lung fuction. | Therapy includes in-halations and physiotherapy, high caloric diet and certain drugs. |
Severe combined immunodeficiency Absence of both humoral and cellular immunity 1:50.000 | PCR-amplification of T-cell receptor excision circles (TRECs), TRECs copy umber | Infants with SCID die of infections by age 2 years unless immunity is reconstituted by Treatment. | Therapy: marrow/steam cell transplantation. Early detection and treatment can result in markedly improved survival rates. |
Expanded Screening by Tandem Mass Spectroscopy
Condition (Incidence) | Symptoms if not treated | Treatment |
Selected Amino acid disorders, amenable to screening Phenylketonuria and Hyperphenylalaninemia (deficiency of phenylalanine hydroxylase activity) (1: 8,000) Maple Syrup Urine Disease (1:100.000) Tyrosinemia I (1:50.00) |
Mental retardation and/or neurological complications. Leading to progressive mental retardation and seizures. Causes mental retardation, physical diabilities and death
progressiv liver and kidney dysfunction |
Protein restricted diet (Low phenylalanine diet), If found early and has restricted diet, the child will grow and develop normally Dietary therapy/ Medications
nitisinone (Orfadin) and restriction of tyrosine in the diet |
Selected Fatty acid disorders, Main: Medium chain acyl-CoA dehydrogenase deficiency (MCAD) (1:10,000) (enzyme defect in the fatty acid metabolic pathway (use of dietary and stored fat))
Very long chain acyl-CoA dehydrogenase- deficiency (VLCAD) Long chain 3-hydroxyacyl-CoA- dehydro-genase deficiency (LCHAD) Carnitine palmitoyl transferase deficiency type 2 (CPT2) neonatal form, extremely rare Carnitine palmitoyl transferase deficiency type 1 (CPT1) Carnitine/acylcarnitine translocase deficiency (CACT) - neonatal form, extremely rare |
Varying Symptoms, Metabolic crisis when an infant "fasts" (goes for a long period of time without eating, such as during an illness), leads to seizures, failure to breathe, cardiac arrest, encephalopathy and death. |
Information of the parents: The child may never fast. Carnitine supplements, Only to prevent a metabolic crisis from happening, |
Selected Organic acid disorders Glutaric aciduria, type 1 (GA1) Isovaleric acidemia (IVA), lead to accumulation of organic acids in biological fluids (blood and urine)) > 1: 80,000 |
Vomiting, metabolic acidosis, ketosis, dehydration or coma, lactic acidosis, hypoglycemia, failure to thrive, hypotonia, global developmental delay, sepsis |
Dietary therapy/medications. Low protein diets, carnitine or vitamin supplements, avoid fasting |
The goal of newborn screening is to identify infants at risk for disorders. The early identification of these disorders in combination with early intervention measures - can often prevent death, disease and disability.
Ideally, the specimen should be collected between the 36th and 72nd hour of life. Specimens collected when the newborn is less than 36 hours old can only be tested for some disorders. So if the specimen is collected too early, a second specimen collection is required.
The parents have to be informed about the purpose and need for newborn screening.
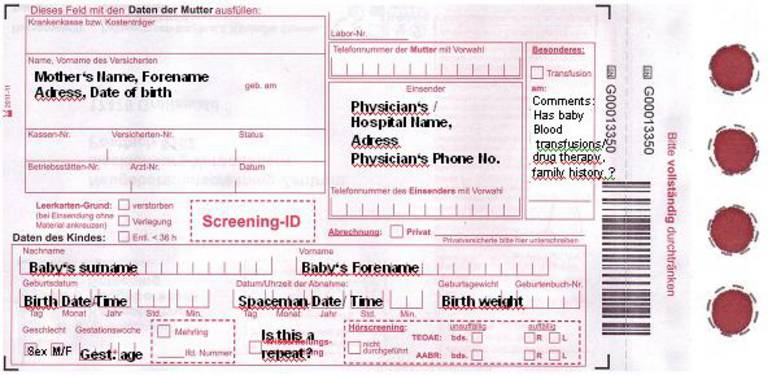
It is very important to fill out the form accurately, legibly and completely. Be sure the correct information of the infant whose blood you are collecting is written on the form. This will help to prevent delays in locating an infant who may need another specimen or require evaluation.
In summary, to obtain the perfect specimen, make sure that the information on the blood collection form is accurate, legible, and complete:
Record the newborn's last name followed by first name. Providing the correct last name for an infant can save valuable time if the baby shows abnormal results.
Use a six-digit number (dd/mm/yy) for date of newborns birth. For example, a baby born on January 2, 2010 would be recorded as 02 01 10. It is very important to correctly enter the infants time of birth correctly because some of the newborn screening test cut-offs are based on how old the infant is at the time of specimen collection.
Use a six-digit number (dd/mm/yy) representing the date on which the specimen was obtained. Accurately record time of specimen collection is very important. Time of collection is used to ensure that the baby was at an appropriate age at the time of specimen collection. Please use the same time method as for the time of birth.
It is important to accurately enter the infants birth weight as some tests have cut-offs based on the infants weight at the time of specimen collection. Please always write the birth weight in grams.
Write an M to designate the newborns gender as male or F to designate the newborns gender as female.
Record the newborns week of gestation at time of birth. It is important that this information is accurate as gestational age does correlate with some analyte levels and can be used to better interpret some results.
Completely shade in the box indicating whether the baby is a multiple. If yes, indicate birth order by filling in the squares labeled 1, 2, or 3.
Completely shade in box to indicate if there are special circumstances that the lab should be aware of when analyzing the specimen. Check the box labeled "Transfused" if the baby was transfused with red blood cells prior to specimen collection. If the baby was transfused, indicate the Date of Transfusion: (dd/mm/yy)
Clinic/Physician/paediatrician that has collecting the specimen.

The primary goal of this standard is to ensure the quality of blood spots collected from newborns. Poor quality specimens place an unnecessary burden on the screening facility, cause unnecessary trauma to the infant and anxiety to the infants parents, potentially delay the detection and treatment of the affected infant, and may contribute to a missed or late diagnosed case. If the Newborn Screening Program receives an unacceptable specimen, program staff requests a repeat sample from the birthing center.
Blood collected from the heel is the standard for newborn screening. The medial and lateral parts of the underfoot are preferred (see diagram on back of newborn screening card).
To begin the collection process, gather your supplies.
You will need: gloves, a soft cloth, sterile alcohol preps, sterile gauze pads, a sterile lancet with a tip that is approximately 2.0 - 2.4 millimeters in depth, the blood collection form.
Warm site with soft cloth,
moistened with warm water up to 41°C,
for three to five minutes.
Cleanse site with alcohol prep.
Wipe DRY with
sterile gauze pad
Puncture heel.
Wipe away first blood
drop with sterile gauze pad.
Allow another LARGE
blood drop to form.
Lightly touch filter paper to LARGE blood drop.
Allow blood to soak through
and completely fill circle with
SINGLE application to LARGE blood drop.
Fill all required circles with blood.
Apply blood to one side of filter paper only.
The specimen should be allowed to air dry in a horizontal position for at least 3 hours
before mailing. Neither side of the blood spots may touch a surface. Specimens are to
be kept away from direct sunlight and heat sources during the drying process. Heat must
not be used to facilitate drying. All specimens must be sent to the laboratory at the day
of collection. Specimens should not be placed in plastic bags prior to mailing!
Adresse: Neugeborenenscreening-Zentrum Mecklenburg-Vorpommern
Postfach 1314
17466 Greifswald
Blood specimen that are not appropriately processed look like follows:




Specimen quantity insufficient for Testing: The filter paper was removed from the drop before the blood
completely filled the circle or soaked through to the other side.
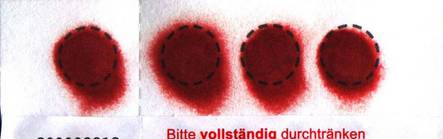
Specimen appears this washed out: Before making skin puncture,
the puncture site was not wiped with alcohol or filter paper was
allowed to come into contact with antiseptic solutions, water, hand lotion
etc., squeezing or milking of area surrounding the puncture side.
If the sample has this insufficient quality, do not wait for the labs call. Blood Specimen Collection has to be repeated immediately.
Follow-up on Requests for Newborn Screening Specimens
Our screening centre informs the physician who collected the sample that an infant has not had newborn screening performed or that an infant needs a repeat specimen. Then it is necessary to obtain the further newborn screening specimen and submit it to the newborn screening centre M-V.
Blood collection on a newborn screening specimen card can be accomplished by sending the infant to the birth hospital laboratory or by collecting the specimen in the clinic.
If our screening centre deems a specimen unsatisfactory for any reason (collected prior to 36 hours of age, layered blood, insufficient quantity of blood to complete testing, spilled substances on the card, etc.) or if an infant shows a borderline result for any assay, the centre may contact the physician directly to request a repeat specimen.
Follow-up on positive newborn screening result
When the screening centre identifies a positive result, the physician/ pediatrician will be immediately notified by phone and fax. A repeat screening card is absolutely essential.
Pediatrician and specialist in together develop a plan of action for necessary diagnostic testing and evaluation, to facilitate appropriate referrals, and to ensure contact with the family to assess the health of the baby and to inform the parents of the need for additional testing and evaluation. Doctors provide support to the parents throughout the process of diagnostic testing and evaluation.
To obtain a purchase/replacement request form to order newborn screening cards, please call/mail us:
Your contact person:
Leiter des Screeningzentrums: Prof. Dr. med. Matthias Nauck